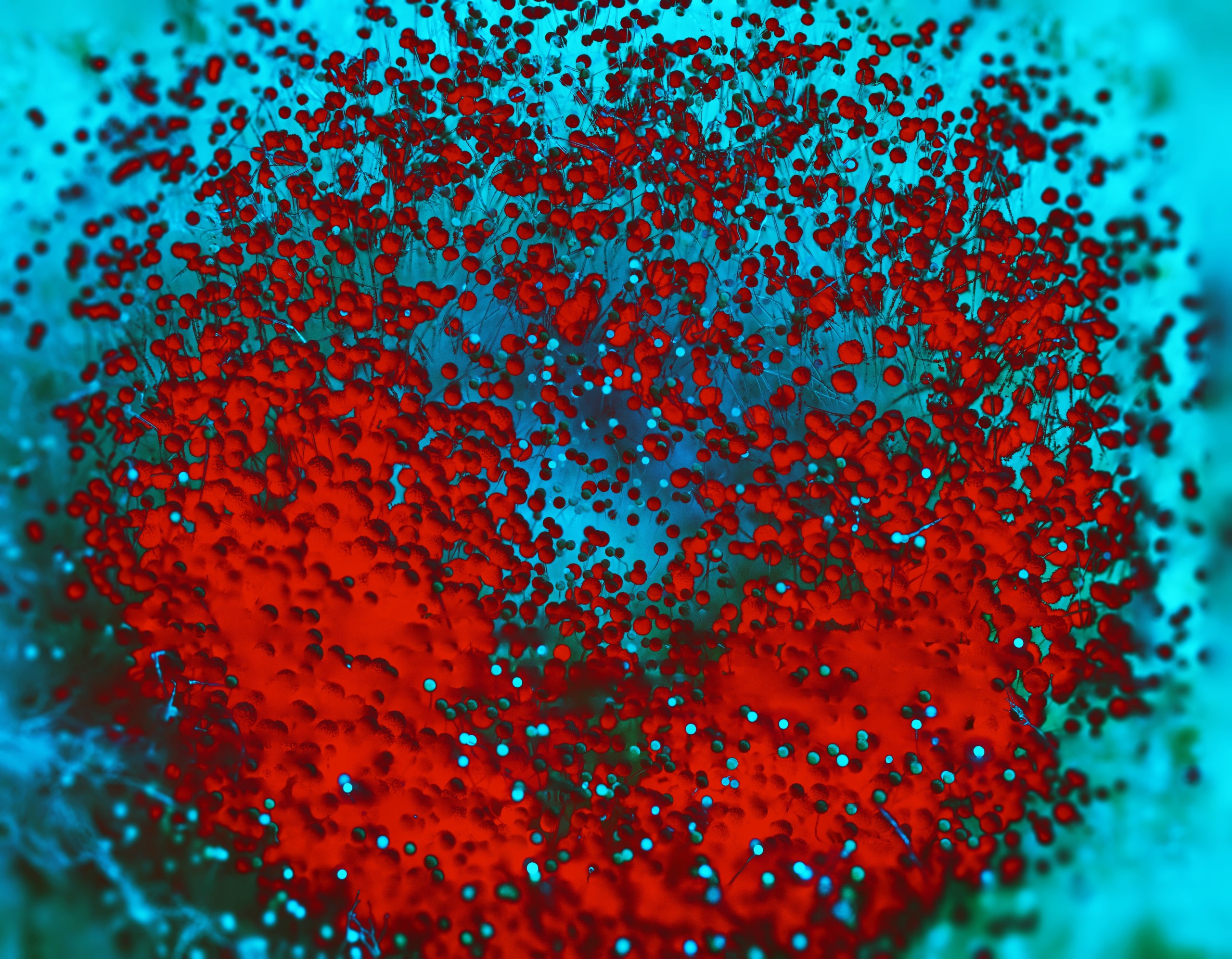
Aspergillus Fumigatus
Aspergillosis are infections due to ubiquitous fungi of the Aspergillus genus. Various pathologies induced depend on several intrinsic characteristics of the fungus itself and on its host, which will condition the virulence of the disease.
Amongst hundreds of Aspergillus species, more than 20 are currently reported to be pathogneous for humans, but new pathogenous species are regularly identified (Gauthier et al., 2016). However, Aspergillus fumigatus is the most commonly encountered species of the genus. It is estimated to be responsible of more than 80% of human pathological manifestations, but this proportion varies depending on clinical forms and geographical location.
A. fumigatus is an opportunistic saprophytic pathogen, naturally present in all kind of environment (soils, air, aquatic habitats, on plants…). Extremely resistant, fungal conidiae penetrates the host mostly by inhalation, but also by ingestion or cutaneous contact through wounds. As they are extremely thin, Aspergillus conidia can reach pulmonary alveolus. After their endocytosis by epithelial cells of the host, they germinate and colonize by dissemination of hyphae, that can reach bloodstream and thus invade other organs (Paulussen et al., 2017).
Clinical manifestations depend on the location of the colonization, which depends on the virulence of the fungus as well as the immune response of the host. Three categories of aspergillosis are distinguished:
- Allergic reactions, including Allergic Broncho-Pulmonary Aspergillosis (ABPA). They are mainly associated with asthma, cystic fibrosis and sinusitis. They correspond to an allergic hyperreactivity to fungi, exacerbated in the case of ABPA by the growth in the pulmonary tract, leading to important inflammation of bronchi (Denning et al., 2014). Besides ABPA, allergic sensitizations are observed, in particular in association with severe asthma, farmer’s lung disease or extrinsic allergic alveolitis due to massive and iterative expositions to the fungus. Allergic forms, particularly ABPA, are responsible for severe respiratory troubles among patients.
- Chronic Pulmonary Aspergillosis (CPA). Different forms are described, but they all correspond to a fungal growth, limited to a fungal ball, or aspergilloma, in the less serious forms, or with tissue invasion, necrosis and bloodstream propagation in the most serious cases. Aspergillus generally grows in a pre-existing cavity due to an underlying or past condition (mostly tuberculosis, but also after obstructive chronic broncho-pneumopathy or Kaposi sarcoma…). Without treatment, except for isolated aspergilloma, the disease has a poor prognosis (Denning et al., 2016).
- Invasive aspergillosis are the most serious forms, affecting immunosuppressed patients (in particular aplastic patients but also those in intensive care). Pulmonary forms are the most common, but disseminated forms are also described (brain, kidney, heart…) (Latgé & Chamilos, 2019). These pathologies are always lethal without treatment, and mortality remains high even with treatment.
Due to its ubiquity, infections by Aspergillus spp. have an important incidence worldwide. It is the first cause of fungal pulmonary infections. Chronic forms have a major impact especially for patients with tuberculosis. The WHO estimates that 22% of patients with pulmonary tuberculosis develop a CPA (Denning et al., 2011). ABPA rate among asthmatic patients is around 2,5%, reaching 7,8% for patients with cystic fibrosis (Kanj et al., 2018). Immunosuppressed patients (AIDS, grafted, hematopoietic diseases…) are at risk, especially for invasive forms, leading to a 40% mortality rate. Overall, twelve million people are suffering of severe asthma with fungal sensitization or ABPA, 3 million of a CPA form and 300.000 of invasive aspergillosis (Bongomin et al., 2017).
The diversity of aspergillosis forms implies a diversity in the diagnostic tools. For invasive aspergillosis, histopathological observation, imaging, culture, fungal DNA detection using PCR and galactomannan detection via ELISA are the most commonly used techniques (Donnelly et al., 2020).
The diagnosis of ABPA relies on a set of criteria including clinical data, total and A. fumigatus specific IgE, radiology and specific IgG (Agarwal et al., 2013). Diagnosis is complex because of the overlapping symptoms between ABPA and underlying conditions, most biological markers do not allow by themselves to discriminate between ABPA, fungal sensitization or a disease for another origin (for instance, due to exposure to another fungus such as Alternaria alternata). Alternative markers, such as the immunologic profile analysis by Western Blot (Piarroux et al., 2019a).
Chronic forms of aspergillosis are diagnosed on the basis of characteristic symptoms and radiology, confirmed by microbiological immunological techniques. In most cases, precipitin or specific IgG presence indicates an Aspergillus infection. Although invasive, biopsies may be interesting, especially for the differential diagnosis of cancers (Kanj et al., 2018).
Serology, essential for the diagnosis of chronic and allergic forms, is done by several techniques. Screening is usually done by ELISA, easily automatable. Confirmation was historically performed by immuno-electrophoresis, but the lack of standardization leads the clinicians to use another technique, like Western Blot (Persat et al., 2017).
SCIENTIFIC REFERENCES
- De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, et al. Revised Definitions of Invasive Fungal Disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis 2008 46 (12): 1813‑21
- Denning DW, Riniotis K, Dobrashian R, Sambakatou H. Chronic Cavitary and Fibrosing Pulmonary and Pleural Aspergillosis: Case Series, Proposed Nomenclature Change, and Review. Clin Infect Dis 2003 37 Suppl 3: S265‑80
- Kwizera R, Katende A, Teu A, Apolot A, Worodria W, Kirenga BJ, Bongomin F. Algorithm-aided diagnosis of chronic pulmonary aspergillosis in low- and middle-income countries by use of a lateral flow device. Eur J Clin Microbiol Infect Dis 2020 Jan ;39(1) :1-3
- Latgé J-P, Chamilos G. Aspergillus fumigatus and Aspergillosis in 2019. Clin. Mic. Rev. 2019 33:e00140-18
- Oliva A, Flori P, Hennequin C, Dubus J-C, Reynaud-Gaubert M, Charpin D, Vergnon JM et al. Evaluation of the Aspergillus Western blot IgG kit for diagnosis of chronic aspergillosis. J Clin Microbiol 2015 53(1):248- 54
- Persat F. Aspergillus serology, from yesterday to today for tomorrow. Journal de Mycologie Médicale, 2012; 22 (1): 72‑82
- Persat F, Hennequin C, Gangneux J-P, SFMM study group. Aspergillus antibody detection: diagnostic strategy and technical considerations from the Société Française de Mycologie Médicale (French Society for Medical Mycology) expert committee. Med Mycol 2017 Apr 1;55(3):302-307
- Piarroux RP, Romain T, Martin A, Vainqueur D, Vitte J, Lachaud L, Gangneux J-P et al.Multicenter Evaluation of a Novel Immunochromatographic Test for Anti-aspergillus IgG Detection. Front Cell Infect Microbiol. 2019; 9: 12
- Richardson MD. Aspergillus serology: Have we arrived yet? Med Mycol 2017 Jan 1;55(1):48-55
- Stuchy-Hunter E. Effect of patient immunodeficiencies on the diagnostic performance of serological assays to detect Aspergillus-specific antibodies in chronic pulmonary aspergillosis [TIMM 2019 symposium 09.1]
- Stucky-Hunter E. Evaluation of the LDBio Aspergillus ICT lateral flow assay as a point-of-care test for serological antibody detection in allergic bronchopulmonary aspergillosis [TIMM 2019 poster 167]
- Stucky-Hunter E, Richardson MD, Denning DW. Evaluation of LD Bio Aspergillus ICT lateral flow assay for IgG and IgM antibody detection in chronic pulmonary aspergillosis. J. Clin. Microbiol. Aug 26;57(9):e00538-19
- Thornton C. Detection of the ‘Big Five’ mold killers of humans: Aspergillus, Fusarium, Lomentospora, Scedosporium and Mucormycetes. Adv Appl Microbiol 2020 ;110 :1-61
- Wilopo BAP, Richardson MD Denning DW. Diagnostic Aspects of Chronic Pulmonary Aspergillosis: Present and New Directions. Cur Fun Inf Rep 2019 13, 292-300
- Zmeili OS, Soubani AO. Pulmonary Aspergillosis: A Clinical Update., QJM: Monthly Journal of the Association of Physicians 2007;100 (6): 317‑34